Acute Respiratory Distress Syndrome (ARDS), pneumonia, and sepsis are common critical illness syndromes inflicting significant morbidity and mortality, both during the acute phase and in the years following the initial illness. Hallmarks of ARDS, pneumonia, and sepsis (APS) include high mortality; complexity of illness; a high burden of pre-existing chronic illness; the possibility of rapid shifts in clinical status; a plethora of adverse events resulting from multiple, simultaneous interventions that can exacerbate and confound the acute disease state; and long-term physical and cognitive morbidity. The presence of significant heterogeneity within each syndrome, combined with the overlapping phenotypes among syndromes, suggests that study of common critical illness syndromes in an interrelated manner may improve the understanding of mechanisms that dictate short- and long-term outcomes and enhance the identification of sub-phenotypes across syndromes.
The goal of the APS Consortium is to support the development of deeper mechanistic understanding of critical illness syndromes to facilitate precision-based therapies that will curtail the devastating morbidity and mortality caused by ARDS, pneumonia and sepsis.
About

The overarching goal of the APS Consortium funded under RFA-HL-23-001 and RFA-HL-23-002 is to support the development of deeper mechanistic understanding of critical illness syndromes to facilitate precision-based therapies that will curtail the devastating morbidity and mortality caused by ARDS, pneumonia and sepsis. To achieve this goal, the consortium will conduct a longitudinal cohort study of adults hospitalized in the United States with ARDS, pneumonia and/or sepsis, and collect multidimensional data and biospecimens during index hospitalization. A subset of patients will be followed up for up to one year. Patient recruitment began in July 2024. These data and biospecimens will be used to complete approved APS studies to enhance our understanding of the mechanistic basis of these syndromes and shared with investigators for potential ancillary studies.
APS Data and Biospecimen Requests:
One of the key objectives of the Consortium is to make the data and biospecimens collected in the APS Consortium available as a resource to the broader research community. Investigators from both inside and outside of the APS Consortium will have equal access to data and biospecimens for the purposes of ancillary studies. APS will consider requests for a letter of support for applications through funding opportunities including but not limited to NOT-HL-21-030 and NOT-GM-24-018.
Timelines:
There are three primary ancillary study proposal submission deadlines throughout the year.
- March 15
- July 15
- November 15
In general, proposals will be processed starting on the first deadline after they are submitted. A proposal may be submitted at any time, but there is no guarantee they will be reviewed outside of these timelines. More information on the submission and review timelines can be found in the Ancillary Study Proposal FAQs linked below in “Resources”.
Submitting ancillary study proposals:
Proposals submission form: https://redcap.link/APSancillary
We strongly encourage interested investigators to read the Ancillary Study Proposal FAQs linked below prior to submitting a proposal. This document includes information on developing proposals, how and when proposals are reviewed, and next steps following review. If you have any further questions prior to submitting a proposal, please email aps_consortium@vumc.org
Specimen collection and availability:
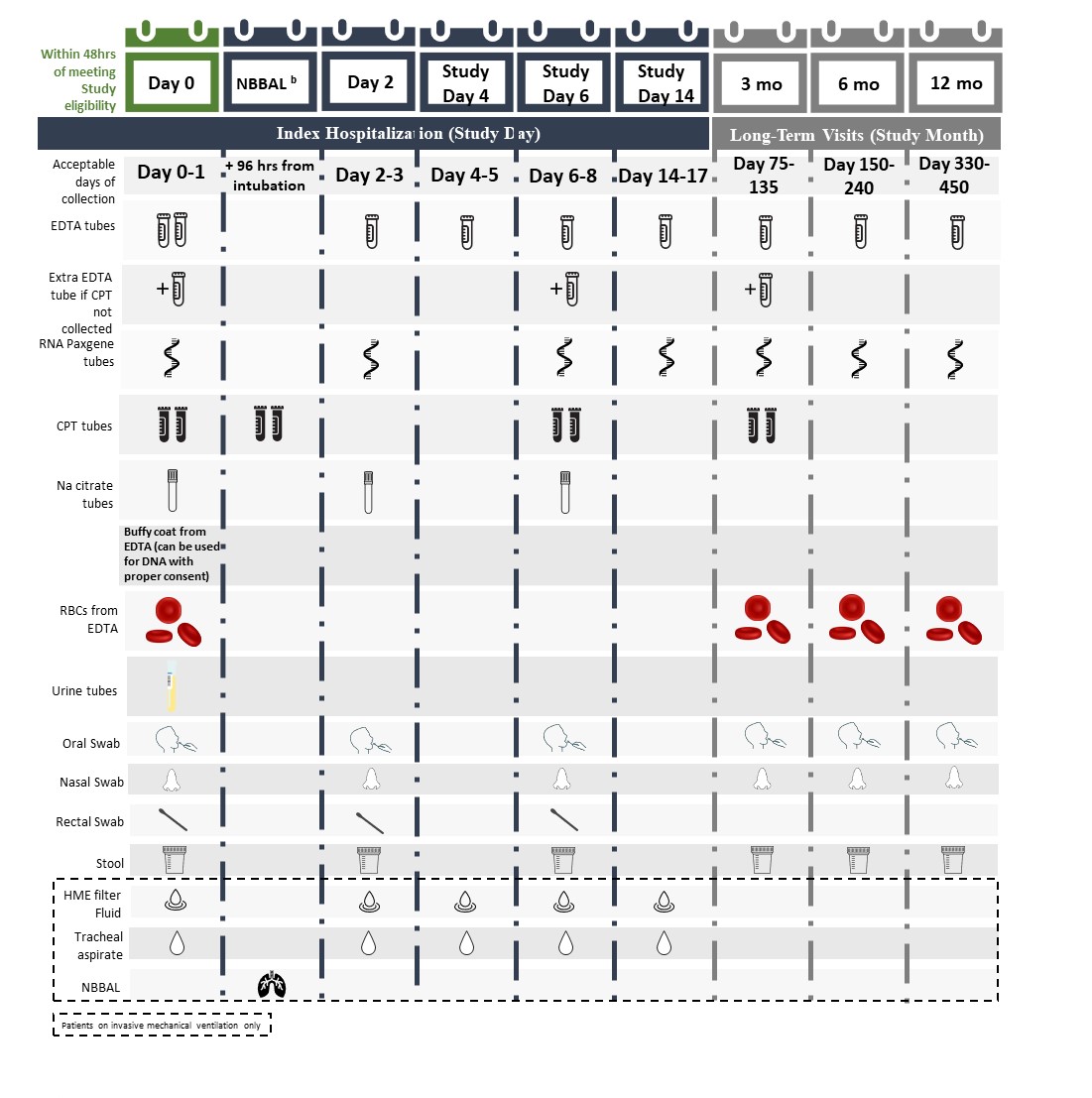
The APS schedule of events including biospecimen types and collection timepoints can be found below. This schedule of events is subject to modifications and may be updated based on study needs and/or feedback from regulatory oversight committees. Subsets of APS data and biospecimens will be released regularly during the enrollment period after meeting appropriate quality control metrics. The first large subset of APS data and biospecimens is anticipated to be available for distribution no earlier than the first quarter of calendar year 2026. Specific requests can be considered earlier. For more immediate access to data and biospecimens in these areas of research, please consider exploring other existing repositories (see BioLINCC or collections mentioned in the report of the Sepsis Human Biospecimens Investigators Meeting). Please check this website for periodic updates on timelines and access to APS data and biospecimens.
Schedule of Events
Resources
- APS Study Protocol A (full protocol), version 5.0
- APS Study Protocol B (alteration of consent), version 5.0
- APS Study Global Consent
- APS Study Part 2 Consent
- APS Study Long Term Outcomes Global Consent
- APS Study Long Term Outcomes Part 2 Consent
- APS Ancillary Study Proposal FAQs
To inquire about access to APS Consortium data and/or biospecimens, please contact aps_consortium@vumc.org for additional information.
Thinking of Participating?
Patient recruitment is expected to begin in 2024.
Study Locations to be determined.

